Pain Management Options
One of the most exhilarating and worthwhile experiences of your life will be the birth of your child. Your obstetrician, anesthesiologist and nurses want to help you, the baby and your partner through this event as safely and pleasantly as possible. Every woman has her own unique labor experience. The amount of pain felt will vary for each woman. It depends on factors such as pain tolerance, size and position of the baby, strength of the uterine contractions and prior birth experiences. Decisions about regulating labor pain must be specific to each woman. Some woman can achieve adequate pain control with the breathing and relaxation techniques learned at child birthing classes but others do not. Many woman are reconsidering the idea that a “natural” childbirth can only be achieved if they suffer through without medication and are choosing pain relief for a more comfortable experience.
Choices for pain relief during labor & delivery
Be assured that your physicians will prescribe or administer medications only in the amounts and during those stages of labor that are best for the safety and well-being of your baby. There are several choices for pain relief:
- Intravenous “I.V.” Medication – Pain relieving medications that are injected into a vein or muscle that will help dull you pain but may not eliminate it completely. These I.V. medications are usually prescribed by your obstetrician. Because they sometimes make both you and your baby feel sleepy, they are used mainly during early labor.
- Local Anesthesia – Other pain relieving medications may be injected in the vaginal and rectal areas by your obstetrician at the time of delivery. These medications are local anesthetics. They provide a numbness or loss of sensation in a small area. Local anesthesia is often used to ease the pain of delivery or when an episiotomy incision is done to assist the delivery. It does not, however, lessen the pain of contractions.
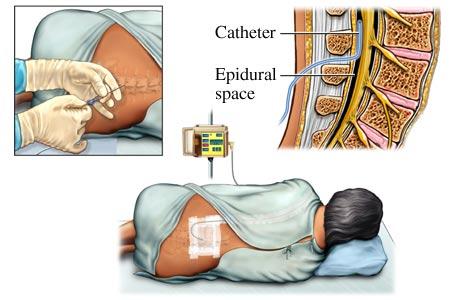
- Epidural Blocks – This block can reduce the discomfort of labor. They are administered in the lower back by an anesthesia provider. Local anesthetics and either drugs are used for these procedures to reduce pain and other sensations to the lower body. Epidurals may be used for labor and delivery and/or cesarean deliveries.
- Subarachnoid Blocks – “spinal” may be used for cesarean delivery.
- Nitrous Oxide – This is a mixture of 50% nitrous gas and 50% oxygen that is inhaled through a mask or mouthpiece that a woman holds and self-administers, as she wishes. A version of nitrous oxide is used widely in dental offices, where most people know of it as “laughing gas”. The blend that is used in laboring women is different, and does not have the same effect, as it is not anesthesia.
Regional blocks for labor
Labor and delivery epidurals are increasingly popular because they provide for a more comfortable experience. The epidural block has the ability to desensitize the lower areas of the body while leaving the patient conscious. When to administer the epidural block for each patient will vary. If you request an epidural block, the obstetrician and anesthesiologist will evaluate you and your baby’s health, the progress of labor, and the baby’s responses and past anesthetic experiences to determine your individual situation.
Questions & Answers
Q: How is the epidural block performed?
A: The epidural block is administered in the lower back below the level of spinal cord. It is given while the patient is either sitting up or laying to the side. The block could also be given in the tailbone area called a caudal block. First, the skin will be cleansed with an antiseptic solution. The anesthesiologist will then use local anesthesia to numb the area near the tailbone on the lower part of the back. The block is performed with a special needle being placed in the epidural space outside the spinal sac. An epidural catheter, a tiny flexible tube, is inserted through the needle. Occasionally, the catheter touches a nerve sending brief tingling sensations down one leg. When the catheter is situated, the needle is removed and the catheter is taped in place. This process allows for additional medications to be given throughout the experience and allows continual pain blocking as the nerves are numbed. This produce sepidural analgesia.
Q: How soon will the epidural block take?
A: The onset of pain relief with an epidural block is gradual because it needs to be absorbed into several nerves. The effect will take within 10-20 min after being injected to numb the area.
Q: What will I feel after the block takes effect?
A: Considerable pain relief will occur, but pressure or sensations from contractions may still be noticeable. Some women feel the obstetrician’s examinations as labor progresses. Depending on each mother and baby’s circumstances, the anesthesiologist adjusts the numbness for comfort and to assist labor and delivery. Some woman even notice a degree of temporary numbness, heaviness or weakness in their legs.
Q: How long will the block last?
A: The epidural analgesia can be extended for as long as you need it. Once the epidural catheter is in place, additional medication can be administered as needed. An anesthesiologist and nurse will monitor your comfort and progress throughout your labor and adjust medications accordingly. After delivery, the catheter is removed and sensations return to normal within a few hours.
Q: Will the epidural affect my baby?
A: Research has shown that both mother and baby can be safe with the use of epidural analgesia and anesthesia with little to no effect on the infant. However, a qualified anesthesiologist should perform this procedure because of the importance of special medical training and judgment, precautions and treatments involved.
Q: Will it slow down my labor?
A: Epidural medications have various effects on different people. Some mothers may feel a brief period of decreased uterine contractions. Many, however, are pleasantly surprised to learn that once the epidural medications have relaxed them, they are more comfortable and their labor actually can progress faster.
Q: Can I “push” when needed?
A: Epidurals allow you to rest during the longest part of labor, which occurs during cervical dilation.
Q: When is general anesthesia used?
A: General anesthesia is used when a regional block is not possible or is not the best choice for medical or other reasons. It can be started instantaneously and causes a rapid loss of consciousness. This is the procedure used when an urgent vaginal or cesarean delivery is required, as in rare instances of problems with the baby or vaginal bleeding. In these circumstances, general anesthesia is quite safe for the baby. The main concern during general anesthesia is if there is food or liquids in the mother’s stomach. During unconsciousness, “aspiration” can occur, meaning that some stomach contents come up and go into the lungs. In the lungs, they could possibly cause pneumonia. Anesthesiologists take extra precautions to protect the lungs, such as placing a breathing tube in the mouth and windpipe after anesthetized. Before a cesarean delivery, the mother may be given and antacid to neutralize the stomach acid. Remember, DON’T EAT OR DRINK ANYTHING AFTER LABOR PAINS BEGIN, regardless of delivery plans or pain control. Sometimes during labor, small sips of water, clear liquids or ice chips are permissible with the physician’s consent.
Q: Will I receive a separate bill from the anesthesiologist?
A: An anesthesiologist is a physician specialist like an obstetrician or pediatrician whose medical services have been requested. It is probable that a separate bill will be received specifically for the anesthesiologist’s professional service as would be true for other physicians. If you have any financial concerns, your anesthesiologist or an office staff member will answer your questions. Note that your hospital charges separately for medications and equipment used.
Options
Modern anesthesiology offers today’s mothers a variety of options for more comfortable childbirth. The anesthesiologist's goal is to answer questions, ease fears and make the labor and delivery experience as safe as possible for your baby. Please discuss any anesthesia-related questions or concerns with your obstetrician. Usually, a consultation with an anesthesiologist can be arranged before your delivery. The more prepared you are –in other words, the more time spent “planning for the childbirth” – the more comfortable and memorable the birth of your baby will be!
