Birth Day
Labor
Whether you’re experiencing a normal pregnancy or a high-risk pregnancy, Guadalupe Regional Medical Center Labor and Delivery has the advanced technology and experienced staff to provide you with superior care.
Before and during labor you can expect the following from GRMC’s Birthing Center:
- A welcoming and relaxing environment in our waiting room
- Experienced staff providing you support and education as you progress in labor
- Highly skilled nurses monitoring your labor and keeping your physician informed of your progress
- Family Centered Care – meaning we keep your baby with you as often as possible
- Strong lactation support, including skin-to-skin for parents and baby
- Expert team to care for your baby
Items to bring when you come to deliver:
- Driver’s license/ID, insurance information and any other hospital paperwork
- Robe and nightgown
- Slippers or non-skid socks
- Nursing bra
- Toiletries
- Flip flops to wear home if your feet are swollen
- Extra bag for additional items to take home
- Camera/phone & charger
- Ponytail holder or hair band
- Going-home outfit for mom and baby
- Installed car seat
- Anything else that you feel will make your stay more comfortable
Signs of Labor
Strong and regular contractions. Although you may experience contractions on and off for several weeks before delivery (known as false labor or Braxton-Hicks contractions), you’re really in labor when:
- Your contractions are consistently 5-10 minutes apart.
- Your contractions are so strong you can’t walk or talk during them.
- You feel pain in your belly and lower back.
- The pain doesn’t go away when you move or change positions.
Water breaking: You may experience your water breaking as a rush of fluid or just a trickle. For many women, their water does not break until later in their labor after they have arrived at the hospital.
Bloody show: A bloody (brownish or reddish) mucus discharge is another sign that labor is beginning.
If you think you’re in labor, call your health care provider, no matter what time of day or night. Your provider can tell you if it’s time to head for the hospital.
Triage
Our Birthing Center offers a beautiful, brand new 4 bed triage for outpatient care. The triage area is utilized for screening patients’ labor status, as well as caring for patients who are visiting for outpatient obstetric care prior to being in labor. The triage area has direct access to our Birthing Center unit and our operating rooms should your status require you to be admitted for the delivery of your baby.
Upon arrival to the triage area, you will be greeted by a highly qualified Registered Nurse (RN) and shown to a private bed. Your RN will be in contact with your obstetrician to assure that you receive the best care possible.
Pain Relief Methods of Labor
- Birthing Ball – GRMC has two birthing balls available for use.
- Peanut Ball – GRMC has two peanut balls available for use. This will help mom by opening up her hips and allowing baby to progress to birth canal.
- Patterned Breathing – Breathing techniques provide comfort and focus while enhancing labor progress.
- Movement and Position Changes – Moving about during labor is usually more comfortable than staying still and can help labor progress by the simple effects of gravity and the changing shape of the pelvis.
- Superficial Heat and Cold – Heat can be effective when applied by using hot moist towels, or warm blankets. While cold can come from an ice bag or washcloths soaked in ice water.
- Counter-Pressure – Steady, strong force applied to one spot on the lower back during contractions. This helps alleviate back pain during labor, especially in those women experiencing “back labor”.
- Touch and Massage – Touch or massages can convey pain-reducing messages.
- Aromatherapy – Aromatherapy is the use of essential oils such as lavender, rose, chamomile, and sage.
- Focus and Distraction – Methods of coping with pain rely on the ability to focus and use mind-diverting activities.
- Audio-Analgesia – Music creates a peaceful and relaxing environment and aids in relaxation. Carefully chosen music can also reinforce rhythmic breathing patterns.
Pain Management Options
One of the most exhilarating and worthwhile experiences of your life will be the birth of your child. Your obstetrician, anesthesiologist and nurses want to help you, the baby and your partner through this event as safely and pleasantly as possible. Every woman has her own unique labor experience. The amount of pain felt will vary for each woman. It depends on factors such as pain tolerance, size and position of the baby, strength of the uterine contractions and prior birth experiences. Decisions about regulating labor pain must be specific to each woman. Some woman can achieve adequate pain control with the breathing and relaxation techniques learned at child birthing classes but others do not. Many woman are reconsidering the idea that a “natural” childbirth can only be achieved if they suffer through without medication and are choosing pain relief for a more comfortable experience.
Choices for pain relief during labor & delivery
Be assured that your physicians will prescribe or administer medications only in the amounts and during those stages of labor that are best for the safety and well-being of your baby. There are several choices for pain relief:
- Intravenous “I.V.” Medication – Pain relieving medications that are injected into a vein or muscle that will help dull you pain but may not eliminate it completely. These I.V. medications are usually prescribed by your obstetrician. Because they sometimes make both you and your baby feel sleepy, they are used mainly during early labor.
- Local Anesthesia – Other pain relieving medications may be injected in the vaginal and rectal areas by your obstetrician at the time of delivery. These medications are local anesthetics. They provide a numbness or loss of sensation in a small area. Local anesthesia is often used to ease the pain of delivery or when an episiotomy incision is done to assist the delivery. It does not, however, lessen the pain of contractions.
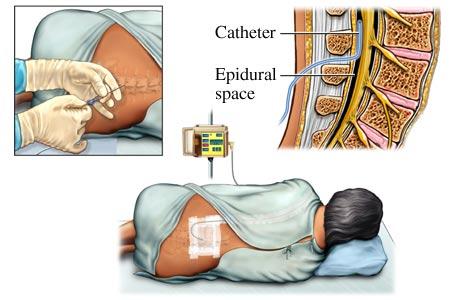
- Epidural Blocks – This block can reduce the discomfort of labor. They are administered in the lower back by an anesthesia provider. Local anesthetics and either drugs are used for these procedures to reduce pain and other sensations to the lower body. Epidurals may be used for labor and delivery and/or cesarean deliveries.
- Subarachnoid Blocks – “spinal” may be used for cesarean delivery.
- Nitrous Oxide – This is a mixture of 50% nitrous gas and 50% oxygen that is inhaled through a mask or mouthpiece that a woman holds and self-administers, as she wishes. A version of nitrous oxide is used widely in dental offices, where most people know of it as “laughing gas”. The blend that is used in laboring women is different, and does not have the same effect, as it is not anesthesia.
Regional blocks for labor
Labor and delivery epidurals are increasingly popular because they provide for a more comfortable experience. The epidural block has the ability to desensitize the lower areas of the body while leaving the patient conscious. When to administer the epidural block for each patient will vary. If you request an epidural block, the obstetrician and anesthesiologist will evaluate you and your baby’s health, the progress of labor, and the baby’s responses and past anesthetic experiences to determine your individual situation.
Questions & Answers
Q: How is the epidural block performed?
A: The epidural block is administered in the lower back below the level of spinal cord. It is given while the patient is either sitting up or laying to the side. The block could also be given in the tailbone area called a caudal block. First, the skin will be cleansed with an antiseptic solution. The anesthesiologist will then use local anesthesia to numb the area near the tailbone on the lower part of the back. The block is performed with a special needle being placed in the epidural space outside the spinal sac. An epidural catheter, a tiny flexible tube, is inserted through the needle. Occasionally, the catheter touches a nerve sending brief tingling sensations down one leg. When the catheter is situated, the needle is removed and the catheter is taped in place. This process allows for additional medications to be given throughout the experience and allows continual pain blocking as the nerves are numbed. This produce sepidural analgesia.
Q: How soon will the epidural block take?
A: The onset of pain relief with an epidural block is gradual because it needs to be absorbed into several nerves. The effect will take within 10-20 min after being injected to numb the area.
Q: What will I feel after the block takes effect?
A: Considerable pain relief will occur, but pressure or sensations from contractions may still be noticeable. Some women feel the obstetrician’s examinations as labor progresses. Depending on each mother and baby’s circumstances, the anesthesiologist adjusts the numbness for comfort and to assist labor and delivery. Some woman even notice a degree of temporary numbness, heaviness or weakness in their legs.
Q: How long will the block last?
A: The epidural analgesia can be extended for as long as you need it. Once the epidural catheter is in place, additional medication can be administered as needed. An anesthesiologist and nurse will monitor your comfort and progress throughout your labor and adjust medications accordingly. After delivery, the catheter is removed and sensations return to normal within a few hours.
Q: Will the epidural affect my baby?
A: Research has shown that both mother and baby can be safe with the use of epidural analgesia and anesthesia with little to no effect on the infant. However, a qualified anesthesiologist should perform this procedure because of the importance of special medical training and judgment, precautions and treatments involved.
Q: Will it slow down my labor?
A: Epidural medications have various effects on different people. Some mothers may feel a brief period of decreased uterine contractions. Many, however, are pleasantly surprised to learn that once the epidural medications have relaxed them, they are more comfortable and their labor actually can progress faster.
Q: Can I “push” when needed?
A: Epidurals allow you to rest during the longest part of labor, which occurs during cervical dilation.
Q: When is general anesthesia used?
A: General anesthesia is used when a regional block is not possible or is not the best choice for medical or other reasons. It can be started instantaneously and causes a rapid loss of consciousness. This is the procedure used when an urgent vaginal or cesarean delivery is required, as in rare instances of problems with the baby or vaginal bleeding. In these circumstances, general anesthesia is quite safe for the baby. The main concern during general anesthesia is if there is food or liquids in the mother’s stomach. During unconsciousness, “aspiration” can occur, meaning that some stomach contents come up and go into the lungs. In the lungs, they could possibly cause pneumonia. Anesthesiologists take extra precautions to protect the lungs, such as placing a breathing tube in the mouth and windpipe after anesthetized. Before a cesarean delivery, the mother may be given and antacid to neutralize the stomach acid. Remember, DON’T EAT OR DRINK ANYTHING AFTER LABOR PAINS BEGIN, regardless of delivery plans or pain control. Sometimes during labor, small sips of water, clear liquids or ice chips are permissible with the physician’s consent.
Q: Will I receive a separate bill from the anesthesiologist?
A: An anesthesiologist is a physician specialist like an obstetrician or pediatrician whose medical services have been requested. It is probable that a separate bill will be received specifically for the anesthesiologist’s professional service as would be true for other physicians. If you have any financial concerns, your anesthesiologist or an office staff member will answer your questions. Note that your hospital charges separately for medications and equipment used.
Options
Modern anesthesiology offers today’s mothers a variety of options for more comfortable childbirth. The anesthesiologist's goal is to answer questions, ease fears and make the labor and delivery experience as safe as possible for your baby. Please discuss any anesthesia-related questions or concerns with your obstetrician. Usually, a consultation with an anesthesiologist can be arranged before your delivery. The more prepared you are –in other words, the more time spent “planning for the childbirth” – the more comfortable and memorable the birth of your baby will be!
Delivery
The Birthing Center at GRMC has been nationally recognized by Healthgrades as being a 5-Star Recipient for vaginal delivery care 6 years in a row! We are honored that GRMC’s Birthing Center has been acknowledged on a national level and we continue to make it our goal to provide a family-centered environment that delivers a safe and pleasant childbirth experience!
While delivering your baby at our Birthing Center, you can expect:
- A welcoming and relaxing environment in our waiting room
- Experienced staff providing you support and education as you progress in labor
- Highly skilled nurses monitoring your labor and keeping your physician informed of your progress
- Family Centered Care – meaning we keep your baby with you as often as possible
- Strong lactation support, including skin-to-skin for parents and baby
- Expert team to care for your baby
- And much more
We also offer two operating room (OR) C-Section Suites, which are located inside the Birthing Center, so you are always in close proximity to an operating room should you need a c-section. You can feel at ease knowing that you will keep the same nursing staff during your c-section that you had while in the Birthing Center.
Types of Births
Giving birth is a very personal experience, and every woman has a unique vision for her journey – with her own preferences and needs. You can feel confident knowing you are in the hands of a skilled team of clinicians and staff.
Unmedicated, Natural Childbirth
Many women choose unmedicated, natural childbirth. Our nurse-midwives work with expectant mothers to find alternative ways to help them cope with pain during labor and delivery. Alternative pain management options include breathing techniques, hypnotherapy, aromatherapy, therapeutic use of music, massage therapy and hydrotherapy.
C-Section
A cesarean birth is the delivery of a baby through an incision made through the mother’s lower abdomen and uterus. This method typically is not a choice for mothers, but rather a medical necessity to safely deliver her baby. Called a cesarean section, or C-section, can be a life-saving technique for both moms and babies. Because cesarean section is a type of surgery, it requires many medical interventions and has the similar risks as other surgeries. In addition, it generally requires additional time in the hospital and increases recovery time and risk for infections.
Maternity Services Pricing Plan
Whether you’re expecting your first child or looking forward to another, it’s the special touches that will make your baby’s birth memorable. GRMC’s new Maternity Services Department is now open and combines state-of-the-art technology with spacious and luxurious private rooms and amenities. Our Maternity Services floor has large labor and delivery rooms and dedicated C-section suites that allow our experienced physicians, specially-trained nurses and support staff to provide mother and baby with expert medical care and emotional support during labor, birth and postpartum stay.
When making a decision where your baby will be delivered, you may be wondering how to finance the birth of your child. While GRMC accepts most major insurances, we also understand that maternity care may not be covered. Therefore, GRMC is pleased to announce a new, discounted “Maternity Services Pricing Plan” for families without maternity or traditional health insurance coverage. Qualified, uninsured families may be eligible for this “Maternity Services Pricing Plan” if payment is made in full by the time of the mother’s discharge.
This plan is designed for a normal, uncomplicated delivery at GRMC and for the routine care mother and baby receives during hospitalization. These discounted prices are not offered to families with Medicaid or other maternity insurance coverage. Any special amenities or accommodations may be subject to additional fees.
Please note: There may be other charges depending on the length of your stay, multiple births, or other services you may request. If your baby needs a higher level of care or additional services, additional financial arrangements can be made. The special Maternity Services Pricing does not include physician fees (obstetrician, family practice, pediatrician, neonatologist, anesthesiologists, or radiologist).
Special maternity services pricing:
- Vaginal Delivery – $2800 (2 day stay); $800 per day* thereafter
- Tubal Ligation during a Vaginal Delivery stay: $1400 (in addition to the $2800 VD charge)
- Cesarean Section Delivery – $4200 (3 day stay); $800 per day* thereafter
- Tubal Ligation with Cesarean Section: included with C-section price.
*A day is defined as staying past midnight. The daily rate is limited to a max of 5 days. For stays past 5 days, additional financial arrangements can be made.
You may pay your package rate in either one lump sum or on a payment plan as long as the total is paid in full by the time of your discharge. If not paid in full, by discharge, the special rate no longer applies.
Payments may be made by cash, check or MasterCard/Visa. If your baby must remain in our care for longer than you are here, then those fees are due at the time of discharge. If you pre-pay for a vaginal delivery and require a Cesarean section, you will be asked to pay the difference (noted above) prior to your discharge. Please contact GRMC’s financial counselor at 830.401.7445, for additional questions about this program or to set up a program package.
Postpartum & Discharge
Congratulations! You have welcomed a new baby into the world. You can expect to be discharged between 24 and 48 hours after giving birth. At GRMC, you can relax knowing you will receive the support and quality care you need to help adjust to changes that will take place.
We highly encourage your baby to stay with you during your time at our Birthing Center and encourage you to hold your baby, skin-to-skin, throughout your time here. Babies kept near their mother tend to feed and sleep better, cry less, and remain healthier overall. Additionally, keeping your baby with you will allow you to learn your babies cues and help you feel more confident when going home.
Birth Certificate Worksheets
This birth certificate worksheet is a tool to help Guadalupe Regional Medical Center collect the necessary information for reporting births in TxEVER, the Texas Electronic Vital Events Registrar. The information you report in TxEVER is used to create a child’s birth certificate. Ensure the information you report is correct so that an accurate birth certificate is created. The birth certificate is a legal document that the child will use throughout their life to prove their identity, birthplace, and parentage. The State of Texas safeguards against the unauthorized release of identifying information from birth certificates to protect the confidentiality of parents and their child.
When you click these links, you'll be directed to GRMC's website (grmedcenter.com) to complete the forms.
Online Birth Certificate Worksheet – English
Online Birth Certificate Worksheet – Spanish
Continuing Care & Boarding
Our Birthing Center is equipped with a state of the art Continuing Care Nursery. Should your baby require additional support at birth, we have a separate 2-bed Continuing Care Nursery where they will be cared for by our highly skilled nursing staff as well as our in-house neonatologist or one of our pediatricians. We understand the importance of bonding with your newborn and should your newborn need to stay for continuing care, we will offer you the option of a complimentary stay in your room after discharge so that you can be close to them at all times.
Breastfeeding
Breastfeeding is a wonderful way to feed and bond with your baby and can provide many benefits. Research shows that breast milk contains the perfect balance of vitamins, protein and fat that your baby needs to grow. Breast milk contains antibodies that help your baby’s immune system to fight off viruses and bacteria. Being breastfed decreases the risk of common and life-threatening infections, asthma and allergies in the first year, and can also reduce the risk of sudden infant death syndrome (SIDS).
The American Academy of Pediatrics recommends exclusive breastfeeding for six months, followed by continued breastfeeding as solid foods are introduced, with continuation of breastfeeding for one year or longer as desired by mom and baby.
Newborn Screening Tests
Each newborn baby is carefully checked at birth for signs of problems or complications. The healthcare provider will do a complete physical exam that includes every body system. Throughout the hospital stay, doctors, nurses, and other healthcare providers continually look at the health of the baby. They are watching for signs of problems or illness. Assessments may include the following:
Apgar Scoring
The Apgar score helps find breathing problems and other health issues. It is part of the special attention given to a baby in the first few minutes after birth. The baby is checked at 1 minute and 5 minutes after birth for heart and respiratory rates, muscle tone, reflexes, and color.
Each area can have a score of 0, 1, or 2, with 10 points as the maximum total. Most babies score 8 or 9, with 1 or 2 points taken off for blue hands and feet because of immature circulation. If a baby has a difficult time during delivery and needs extra help after birth, this will be shown in a lower Apgar score. Apgar scores of 6 or less usually mean a baby needs immediate attention and care.
Birth weight
A baby’s birth weight is an important marker of health. Full-term babies are born between 37 and 41 weeks of pregnancy. The average weight for full-term babies is about 7 pounds (3.2 kg). In general, very small babies and very large babies are at greater risk for problems. Babies are weighed every day in the nursery to look at growth, and the baby’s need for fluids and nutrition. Newborn babies may often lose 5% to 7% of their birth weight. This means that a baby weighing 7 pounds, 3 ounces at birth might lose as much as 8 ounces in the first few days. Babies will usually gain this weight back within the first 2 weeks after birth. Premature and sick babies may not begin to gain weight right away.
Measurements
The hospital staff takes other measurements of each baby. These include:
- Head circumference – This is the distance around the baby’s head.
- Chest Circumference – This is the distance around the baby’s chest.
- Length – This is the measurement from top of head to the heel.
The staff also checks these vital signs:
- Temperature – This checks that the baby is able to have a stable body temperature in a normal room environment.
- Pulse – A newborn’s pulse is normally 120 to 160 beats per minute.
- Breathing rate – A newborn’s breathing rate is normally 40 to 60 breaths per minute.
Physical Exam
A complete physical exam is an important part of newborn care. The healthcare provider carefully checks each body system for health and normal function. The provider also looks for any signs of illness or birth defects. Physical exam of a newborn often includes:
- General appearance – This looks at physical activity, muscle tone, posture, and level of consciousness.
- Skin – This looks at skin color, texture, nails, and any rashes.
- Head and neck – This looks at the shape of head, the soft spots (fontanelles) on the baby’s skull, and the bones across the upper chest (clavicles).
- Face – This looks at the eyes, ears, nose, and cheeks.
- Mouth – This looks at the roof of the mouth (palate), tongue, and throat.
- Lungs – This looks at the sounds the baby makes when they breathe. This also looks at the breathing pattern.
- Heart sounds and pulses in the groin (femoral)
- Abdomen – This looks for any masses or hernias.
- Genitals and anus – This checks that the baby has open passages for urine and stool.
- Arms and legs – This checks the baby’s movement and development.
Gestational Assessment
The healthcare provider will check how mature the baby is. This is an important part of care. This check helps figure out the best care for the baby if the dates of a pregnancy are uncertain. For example, a very small baby may actually be more mature than they appear by size and may need different care than a premature baby needs.
Healthcare providers often use an exam called the Dubowitz/Ballard Examination for Gestational Age. This exam can closely estimate a baby’s gestational age. The exam looks at a baby’s skin and other physical features, plus the baby’s movement and reflexes. The physical maturity part of the exam is done in the first 2 hours of birth. The movement and reflexes part of the exam is done within 24 hours after birth. The provider often uses the information from this exam to help with other maturity estimates.
Physical Maturity
The physical maturity part of the Dubowitz/Ballard exam looks at physical features that look different at different stages of a baby’s gestational age. Babies who are physically mature usually have higher scores than premature babies.
Points are given for each area of assessment. A low of 1 or 2 means that the baby is very immature. A score of 4 or 5 means that the baby is very mature (postmature). These are the areas examined:
- Skin textures – Is the skin sticky, smooth, or peeling?
- Soft, downy hair on the baby’s body (lanugo) – This hair is not found on immature babies. It shows up on a mature infant but goes away for a postmature infant.
- Plantar creases – These are creases on the soles of the feet. They can range from absent to covering the entire foot.
- Breast – The provider looks at the thickness and size of breast tissue and the darker ring around each nipple (areola).
- Eyes and ears – The provider checks to see if the eyes are fused or open. They also check the amount of cartilage and stiffness of the ears.
- Genitals, male – The provider checks for the testes and how the scrotum looks. It may be smooth or wrinkled.
- Genitals, female – The provider checks the size of the clitoris and the labia and how they look.
Maturity of Nerves and Muscles
The healthcare provider does 6 checks of the baby’s nerves and muscles. A score is given for each area. Typically, the more mature the baby is, the higher the score. These are the areas checked:
- Skin textures – This looks at how the baby holds their arms and legs.
- “Square window” – This looks at how far the baby’s hands can be flexed toward the wrist.
- Arm recoil – This looks at how much the baby’s arms “spring back” to a flexed position.
- Popliteal angle – This looks at how far the baby’s knees extend.
- “Scarf sign” – This looks at how far the baby’s elbows can be moved across the baby’s chest.
- Heel to ear – This looks at how near the baby’s feet can be moved to the ears.
When the physical assessment score and the nerves and muscles score are added together, the healthcare provider can estimate the baby’s gestational age. Scores range from very low for immature babies to very high scores for mature and postmature babies.
All of these exams are important ways to learn about your baby’s well-being at birth. By finding any problems, your baby’s healthcare provider can plan the best possible care.
FAQ
What is the visitation policy at the Birthing Center?
- Visiting Hours are from 7am-10pm. All visitors must be free of any signs/symptoms of illness. Children must be accompanied by a supervising adult.
- Visitors are limited to 2 during delivery to allow space for staff and unanticipated emergencies.
- Visitors 12 years of age and over are allowed in the Special Care Nursery. Each visitor must be accompanied by a banded individual.
- Doors to the Birthing Center are kept locked for security purposes. Access is granted to the unit by stating the patient’s first and last name. We ask that visitors do not hold the door open for others.
- Disruptive visitors will respectfully be asked to leave so we can maintain a calm and relaxing environment for our patients and their family.
- The first hour after delivery is known as the “Golden Hour”. This is a special time to bond with your baby and initiate breastfeeding. Visitors will be limited to those present for delivery during this time.
Who can be with me during birth?
You may have two support people over the age of 14 with you during delivery.
Can I eat or drink while in labor?
Unfortunately, you cannot eat or drink, however we can provide you with ice chips to ensure you are hydrated during labor.
What are the photography/videotaping policies during labor & delivery?
Pictures are allowed, however no video is allowed until after the baby is born.
How long is the average stay for new moms and babies?
You can expect to stay 24 to 48 hours after delivery.
What do I pack to bring to the hospital?
You’ll want to pack an extra change of comfortable clothes, toiletries, baby blanket and baby clothes.
Will my baby be able to stay with me throughout the hospital stay?
Yes, as long as the baby is healthy and does not require care from a nurse or doctor.
When are meals served?
- Breakfast: 8:30am – 9:00am
- Lunch: 12:30pm – 1:00pm
- Dinner 5:30pm – 6:00pm
Which newborn tests are performed while my baby is in the hospital?
Newborn tests will include a PKU and Bilirubin, as well as a congenital heart and hearing screening.
Where do I go when I arrive at the hospital to deliver?
You’ll come directly to the Birthing Center, which can be conveniently accessed from the Patient Tower entrance. If it is after hours, you will need to enter through the ER entrance and then come to the Birthing Center.
Where can I park?
Between 7:00am and 9:00pm, you can park in front of the patient tower entrance. Between 9:00pm and 7:00am, park at the ER entrance.
